- Veterinary View Box
- Posts
- Bacterial Meningitis in Dogs: 83% Survival and Favorable Long-Term Outcomes in a Multicenter Case Series
Bacterial Meningitis in Dogs: 83% Survival and Favorable Long-Term Outcomes in a Multicenter Case Series
JVIM 2023
Faye Rawson, Max Foreman, Thomas Mignan, Jack Galer, Anne Fraser, Abbe Crawford
Background
Bacterial meningitis (BM) and bacterial meningoencephalomyelitis (BMEM) are serious inflammatory diseases of the central nervous system associated with high morbidity and mortality in humans, but outcome data in dogs remain limited. Clinical presentation in dogs can be variable, and BM/BMEM may resemble other inflammatory CNS diseases such as steroid-responsive meningitis arteritis. The authors aimed to describe clinical features, diagnostic findings, treatment approaches, relapse frequency, and long-term neurological outcomes in dogs diagnosed with BM/BMEM without empyema.
Methods
This was a retrospective multicenter case series including 24 client-owned dogs diagnosed with BM or BMEM between January 2010 and August 2020 at five UK referral hospitals. Inclusion criteria were based on cerebrospinal fluid (CSF) cytology, culture results, and/or neutrophilic pleocytosis with clinical response to antibiotics. Dogs with imaging evidence of empyema or intracranial abscessation were excluded. Data collected included signalment, clinical signs, laboratory findings, imaging results, CSF analysis, bacteriology, treatment details, and follow-up outcomes.
Results
The median age was 4.2 years, with brachycephalic breeds overrepresented. Clinical signs were most often acute, and neurological deficits were present in 75% of dogs, commonly involving vestibular dysfunction. Pyrexia was infrequently documented. Otitis media/interna was identified as the suspected source of infection in 63% of cases. CSF analysis revealed marked neutrophilic pleocytosis in all dogs, with intracellular bacteria identified in 63%, while CSF cultures were positive in 38%. Twenty dogs (83%) survived to hospital discharge. Median duration of antibiotic therapy was 8 weeks, with shorter courses in surgically managed dogs. Relapse was uncommon, and residual neurological deficits were reported in 47% of dogs with long-term follow-up, typically mild and most often vestibular in nature.
Limitations
The study was retrospective with a small sample size, variable diagnostic and treatment protocols, and incomplete long-term follow-up for all cases. Inclusion of dogs without definitive bacterial isolation raises the possibility that some cases may have had noninfectious inflammatory etiologies. Owner-reported outcomes were subject to recall and reporting bias.
Conclusions
Dogs with BM/BMEM without empyema generally have a favorable prognosis when treated promptly with antibiotics, with most surviving to discharge and many achieving full recovery. Otitis media/interna was the most common infection source, and relapses were rare. Although mild residual neurological deficits were relatively common, overall long-term outcomes were good, supporting aggressive medical and, when indicated, surgical management of this condition.
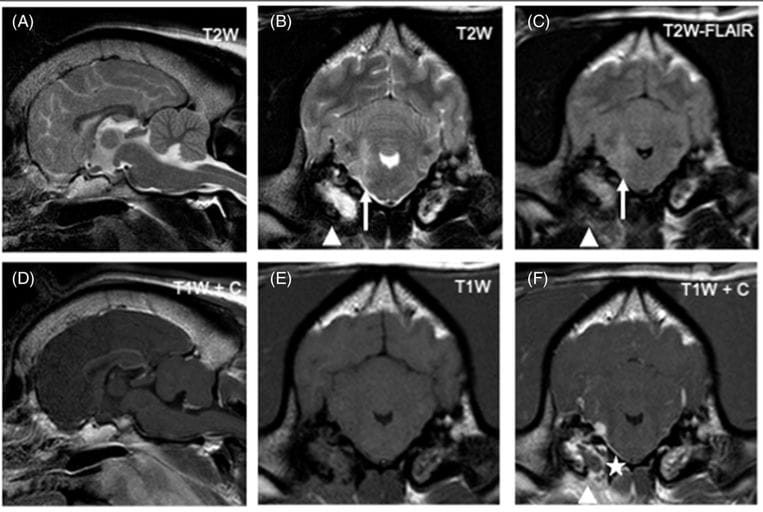
Magnetic resonance images of the head of a dog diagnosed with bacterial meningoencephalitis secondary to otogenic infection (dog 6). From left to right: Top row: sagittal T2W image (A), transverse T2W (B), transverse T2W-FLAIR (C); Bottom row: sagittal T1W postgadolinium (D), transverse T1W pregadolinium (E), transverse T1W postgadolinium administration (F). Transverse images are at the level of the tympanic bullae and, by convention, the right side of the dog is displayed on the left of the image. There is an ill-defined T2W and T2W-FLAIR hyperintensity (compared to normal gray matter) of the right rostral medulla oblongata extending dorsally into the middle cerebellar peduncle (white arrow). The adjacent meninges show contrast enhancement and a focal area of thickening (asterisk). There is bilateral T2W and T2W-FLAIR hyperintensity of the tympanic bullae contents (more pronounced and homogenous on the right), with bilateral contrast enhancement (again more pronounced on the right). Ventral to the right tympanic bulla there is ill-defined T2W and T2W-FLAIR hyperintensity of the soft tissues with marked contrast enhancement (arrowheads)
How did we do? |
Disclaimer: The summary generated in this email was created by an AI large language model. Therefore errors may occur. Reading the article is the best way to understand the scholarly work. The figure presented here remains the property of the publisher or author and subject to the applicable copyright agreement. It is reproduced here as an educational work. If you have any questions or concerns about the work presented here, reply to this email.