- Veterinary View Box
- Posts
- Can Fractional Shortening Reliably Screen Canine Systolic Function?
Can Fractional Shortening Reliably Screen Canine Systolic Function?
Vet Anaesth Analg. 2025
Manuel Martin-Flores; Mark Rishniw
Background
Shortening fraction is widely used in veterinary echocardiography as a simple indicator of left ventricular systolic function, despite its limitations and declining use in human cardiology in favor of volumetric ejection fraction. In dogs, regional wall motion abnormalities are considered uncommon, suggesting that shortening fraction may adequately reflect global systolic function, particularly during abbreviated or preanesthetic examinations. However, the relationship between shortening fraction and ejection fraction, and the diagnostic performance of shortening fraction in identifying normal and abnormal systolic function in dogs, had not previously been systematically evaluated.
Methods
This study reanalyzed prospectively collected echocardiographic data from 224 dogs, including 86 healthy dogs, 96 dogs with mitral valve disease, and 42 dogs with other cardiac pathologies. Ejection fraction was calculated using the Simpson’s method of discs from right parasternal long-axis (RPLA) and left apical four-chamber (LA4C) views, while shortening fraction was measured using M-mode from the right parasternal short-axis view. Measurements were performed by five experienced echocardiographers, averaging three consecutive cardiac cycles. Ejection fraction and shortening fraction were classified as low, normal, or high based on reference intervals derived from the dataset. Sensitivity, specificity, and predictive values of shortening fraction for identifying abnormal ejection fraction were calculated, and relationships between measurements were analyzed using regression methods.
Results
Shortening fraction demonstrated a slightly curvilinear but largely linear relationship with ejection fraction derived from both volumetric views. Sensitivity and specificity of shortening fraction for detecting low ejection fraction were 92% and 93% when ejection fraction was measured from the RPLA view, and 71% and 91% when measured from the LA4C view. Negative predictive values for identifying low ejection fraction were high (97–99%), whereas positive predictive values were lower (46–55%). Overall, shortening fraction showed moderate to high diagnostic performance for identifying low, normal, and high ejection fraction, though its performance was inferior to that of one volumetric method compared against the other.
Limitations
The prevalence of low ejection fraction in the study population was low, which likely reduced positive predictive values. Echocardiographic images were obtained by experienced cardiologists, limiting generalizability to examinations performed by less experienced operators. The study did not evaluate the effects of specific cardiac diseases, loading conditions, or anesthetic drugs on shortening fraction measurements. Additionally, volumetric measurements from different views were not interchangeable, which may have influenced comparative analyses.
Conclusions
Shortening fraction is a robust indicator of ejection fraction in dogs, with high sensitivity and specificity for detecting decreased left ventricular systolic function. Although it has a substantial false-positive rate, its high negative predictive value supports its use as a screening tool to rule out systolic dysfunction, particularly during perianesthetic evaluations when comprehensive echocardiography is not feasible. Despite its limitations, shortening fraction remains a practical and clinically useful parameter in canine cardiac assessment.
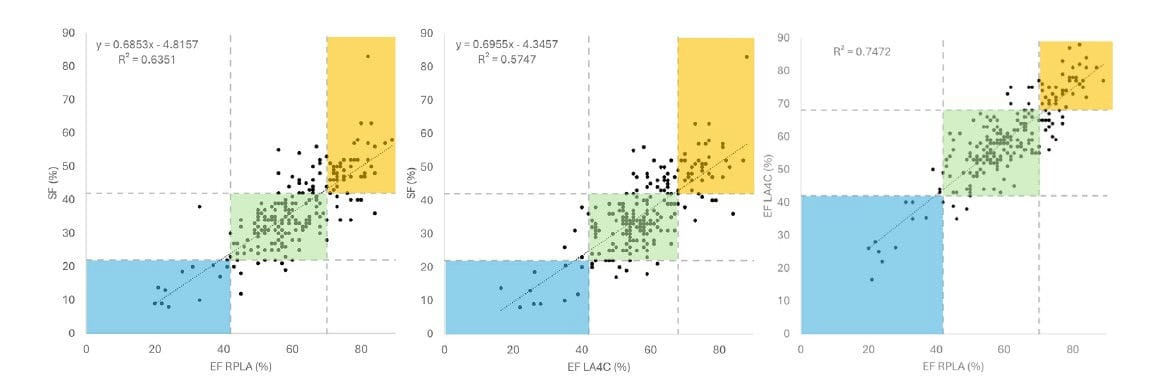
Shortening fraction (SF) values plotted against ejection fraction (EF) obtained from two different views (left and middle), and ejection
fraction values plotted against each other. Data were collected from 224 dogs. Ejection fraction was calculated using the Simpon’s method of discs
and shortening fraction using M-mode. Colored areas represent values of low (light blue), normal (green), or high (yellow) shortening and ejection
fractions. RPLA, right parasternal long axis; RPSA, right parasternal short axis; LA4C, left apical four chamber.
How did we do? |
Disclaimer: The summary generated in this email was created by an AI large language model. Therefore errors may occur. Reading the article is the best way to understand the scholarly work. The figure presented here remains the property of the publisher or author and subject to the applicable copyright agreement. It is reproduced here as an educational work. If you have any questions or concerns about the work presented here, reply to this email.