- Veterinary View Box
- Posts
- Can you help clinician predict survival from acute pancreatitis?
Can you help clinician predict survival from acute pancreatitis?
BMC Veterinary Research 2020
Eleonora Gori, Alessio Pierini, Gianila Ceccherini, Simonetta Citi, Tommaso Mannucci, Ilaria Lippi, Veronica Marchetti
Background
In humans, acute pancreatitis (AP) is frequently associated with respiratory complications, including acute lung injury (ALI) and acute respiratory distress syndrome (ARDS), which contribute to high mortality. However, the prevalence and severity of pulmonary complications in canine AP remain poorly described. This study aimed to (1) assess the prevalence, types, and severity of pulmonary complications in dogs with AP, and (2) evaluate their association with mortality.
Methods
Study Design: Prospective observational study.
Study Population:
-26 client-owned dogs diagnosed with acute pancreatitis based on clinical signs, increased canine pancreatic lipase (cPL), and abdominal ultrasound findings.
-Dogs were categorized as survivors (n = 14) and non-survivors (n = 12).
Pulmonary Evaluation:
-Clinical respiratory assessment (respiratory distress, cyanosis).
-Thoracic radiographs (categorized as normal, interstitial, or alveolar pattern).
-Modified lung injury score (mLIS) to quantify lung abnormalities.
-Arterial blood gas analysis (PaO₂, PaCO₂, bicarbonate levels, A-a gradient).
-Diagnosis of VetALI/VetARDS based on veterinary consensus criteria.
Statistical Analysis:
-Comparison of clinical, radiological, and blood gas parameters between survivors and non-survivors.
-ROC curve analysis to identify predictors of mortality.
Results
Prevalence of Pulmonary Complications:
-80.7% (21/26) of dogs had radiographic lung abnormalities (alveolar: n = 11, interstitial: n = 10).
-46% (12/26) exhibited respiratory distress, which was strongly associated with death (P < 0.001).
-34.6% (9/26) met the criteria for VetALI, while no dogs developed VetARDS.
Comparison Between Survivors and Non-Survivors:
-Higher respiratory rate in non-survivors (55.6 vs. 32 breaths/min, P = 0.006).
-Non-survivors had more severe radiographic abnormalities (P = 0.02).
-Higher mLIS was associated with increased mortality (P = 0.0023).
-Non-survivors had significantly lower PaCO₂ (P = 0.014) and bicarbonate levels (P = 0.019).
-Higher A-a gradient in non-survivors (P = 0.04), indicating impaired gas exchange.
Predictors of Mortality:
-PaCO₂ < 25.25 mmHg had 75% sensitivity and 92.8% specificity for predicting death.
-Bicarbonate < 5.3 mmol/L was associated with 83.3% sensitivity and 85.7% specificity for mortality prediction.
Limitations
Small sample size (n = 26), limiting statistical power.
Lack of follow-up imaging to assess disease progression.
Absence of necropsy confirmation of VetALI, preventing histopathologic correlation.
Conclusions
Pulmonary complications are common in canine AP (80.7%) and significantly impact mortality risk. Respiratory distress, radiographic abnormalities, high mLIS, and arterial blood gas derangements (low PaCO₂, bicarbonate, and increased A-a gradient) were associated with death. VetALI occurred in one-third of dogs with AP, but VetARDS was not observed. Early recognition and monitoring of respiratory complications in dogs with AP is crucial for prognosis and management.
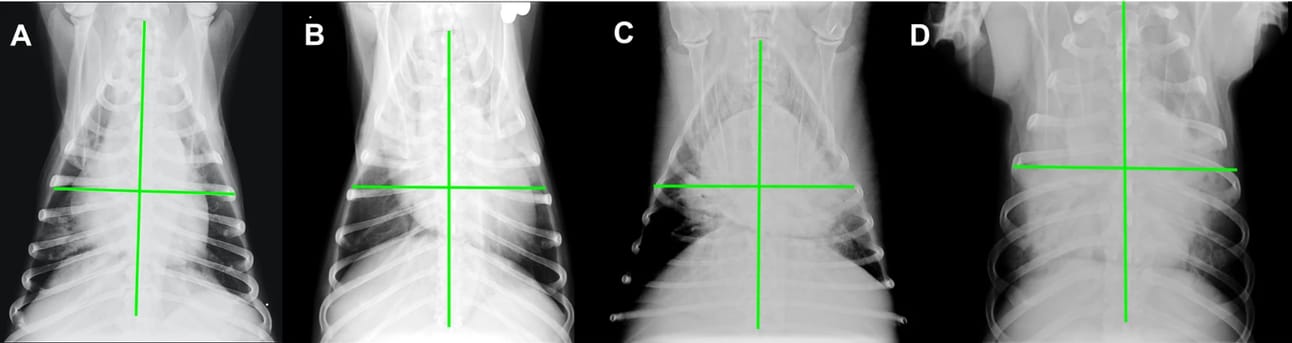
Subdivision of the thorax into four lung quadrants as defined in the modified lung injury score (mLIS). The mLIS was calculated based on how many quadrants were radiographically involved. This figure has to be the one with the single x-ray, which now is Fig. 1
How did we do? |
Disclaimer: The summary generated in this email was created by an AI large language model. Therefore errors may occur. Reading the article is the best way to understand the scholarly work. The figure presented here remains the property of the publisher or author and subject to the applicable copyright agreement. It is reproduced here as an educational work. If you have any questions or concerns about the work presented here, reply to this email.