- Veterinary View Box
- Posts
- DWI Breakthrough: MRI Metric Accurately Identifies Canine Brain Abscesses Among Ring-Enhancing Lesions
DWI Breakthrough: MRI Metric Accurately Identifies Canine Brain Abscesses Among Ring-Enhancing Lesions
Veterinary Radiology & Ultrasound (2025)
Adrien M. Dupanloup, Craig S. Brown, Karen M. Vernau, Ehren M. McLarty, Peter J. Dickinson
Background
Intracranial ring-enhancing lesions are a common but diagnostically challenging MRI finding in dogs and cats, arising from diverse causes such as infection, neoplasia, inflammation, or vascular injury. Conventional MRI sequences often fail to clearly distinguish between these etiologies. Diffusion-weighted imaging (DWI), which assesses water molecule movement, can differentiate restricted from facilitated diffusion, providing microstructural insight. This study aimed to determine whether apparent diffusion coefficient (ADC) values from DWI can distinguish infectious intracranial ring-enhancing lesions from non-infectious ones.
Methods
This retrospective study reviewed 69 cases (68 dogs, 1 cat) with MRI-confirmed intracranial ring-enhancing lesions imaged between 2010 and 2024 using a 1.5 T MRI system. Inclusion required histopathological or microbiological confirmation. Lesions were categorized as intraparenchymal bacterial abscess, extraparenchymal bacterial empyema, fungal abscess, glioma, other neoplasia, non-infectious inflammatory, or vascular. DWI sequences (b = 0, 1000 s/mm²) were used to calculate ADC maps, and normalized ADC ratios (rADC = ADC_lesion/ADC_contralateral brain) were derived. Statistical comparisons employed Kruskal–Wallis and Dunn’s tests, with ROC analysis assessing diagnostic thresholds.
Results
Intraparenchymal bacterial abscesses showed markedly reduced diffusion, with median rADC = 0.54 (0.19–0.82), significantly lower than gliomas (1.7 [0.80–3.9]; p = 0.0003) and non-infectious inflammatory lesions (1.7 [0.74–3.3]; p = 0.024). Extraparenchymal empyemas (rADC = 2.8 [1.3–3.4]) and fungal abscesses (1.2 [1.1–1.8]) did not show restricted diffusion. ROC analysis determined that an rADC < 0.65 (excluding hemorrhagic lesions) had specificity 98% and sensitivity 78% for diagnosing intraparenchymal bacterial abscess. Hemorrhagic lesions also exhibited low ADC values but were distinguishable via T2* or SWI sequences.
Limitations
As a retrospective study, it lacked longitudinal data to assess lesion evolution or treatment effects. The relatively small number of cases per category and absence of interobserver variability analysis may limit generalizability. DWI was acquired with only two b-values, potentially limiting diffusivity characterization, and ROI-based analysis introduced subjectivity.
Conclusions
DWI and ADC mapping are valuable adjuncts to standard MRI for differentiating intraparenchymal bacterial abscesses, which consistently demonstrate restricted diffusion, from gliomas and non-infectious inflammatory lesions. However, extraparenchymal empyemas and fungal abscesses may lack diffusion restriction. Incorporating DWI into MRI protocols enhances diagnostic specificity for ring-enhancing lesions and aids in clinical decision-making regarding infectious versus non-infectious etiologies.
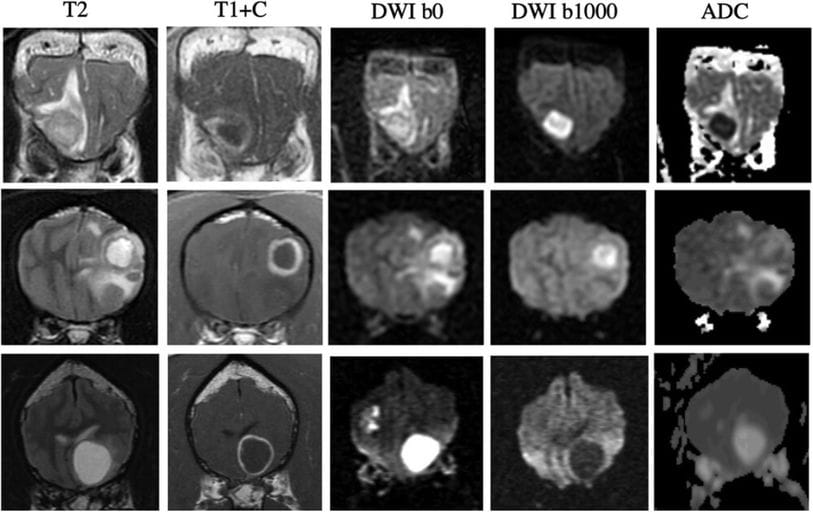
Examples of T2-weighted (T2), T1-weighted post-contrast (T1+C), DWI b0 and b1000, and apparent diffusion coefficient (ADC) map for intraparenchymal infectious lesions and ring-enhancing glioma. Top row: Bacterial abscess. The lesion is hyperintense on DWI b1000 with low signal on the corresponding ADC map, suggestive of marked restricted diffusion. Middle row: Fungal abscess caused by Pheohyphomycosis sp. The lesion is hyperintense on DWI b1000 with high signal on the corresponding ADC map, suggestive of lack of restrictive diffusion. The high signal on DWI b1000 is due to T2-shine-through phenomenon. Bottom row: high-grade oligodendroglioma. The lesion is hypointense on DWI b1000 with high signal on the corresponding ADC map, suggestive of a lack of restricted diffusion.
How did we do? |
Disclaimer: The summary generated in this email was created by an AI large language model. Therefore errors may occur. Reading the article is the best way to understand the scholarly work. The figure presented here remains the property of the publisher or author and subject to the applicable copyright agreement. It is reproduced here as an educational work. If you have any questions or concerns about the work presented here, reply to this email.