- Veterinary View Box
- Posts
- First Young-Dog Case of Optic Pathway Oligodendroglioma Revealed by MRI and Histopathology
First Young-Dog Case of Optic Pathway Oligodendroglioma Revealed by MRI and Histopathology
Vet Ophthalmol. 2025
Vienna M. Lunking, Rajdeep Multani, Devin Fussell, LaTisha N. Knight, Erin Keenihan, Danielle M. Meritet, Abigail R. Armwood, Annie Oh
Background
Gliomas are common primary canine CNS tumors, typically affecting older dogs and brachycephalic breeds. Oligodendrogliomas usually arise from the cerebral hemispheres and rarely involve the optic pathway. Historical pathology collections indicate that optic nerve or retinal oligodendrogliomas are extremely rare, comprising only 0.36% of ocular neoplasms, with only one prior oligodendroglioma reported in the optic nerve or retina. This case report describes the first documented high-grade optic chiasm and bilateral optic nerve oligodendroglioma in a young dog, presented using the revised 2018 canine glioma classification system.
Methods
A 29-month-old German Shepherd with acute bilateral blindness underwent serial ophthalmic examinations, neurologic evaluation, CBC, serum biochemistry, urinalysis, infectious disease testing, anesthetized MRI, ultrasound-guided Tru-cut biopsy of the retrobulbar mass, and complete necropsy. MRI included T2-weighted, T2-FLAIR, T1-FLAIR, SWI, DWI, ADC, and post-contrast T1 sequences. Histopathology and immunohistochemistry (OLIG2, GFAP) were performed on both biopsy and postmortem tissues.
Results
MRI revealed a large, lobulated, extra-axial mass extending from the retrobulbar space through the optic canals into the intracranial vault, compressing the optic chiasm and causing severe left-sided retrobulbar expansion. The mass was hyperintense on T2 and T2-FLAIR, showed mixed T1 signals, and demonstrated marked heterogeneous contrast enhancement with central necrosis, susceptibility artifacts, and meningeal enhancement. Biopsy demonstrated atypical spindle cell proliferation but was inconclusive. Necropsy identified a firm optic pathway mass (approximately 3 cm) effacing the optic nerve and infiltrating retrobulbar musculature and meninges. Histopathology revealed sheets of round neoplastic cells with perinuclear halos, microvascular proliferation, necrosis, and high mitotic activity. OLIG2 showed strong nuclear staining in 40–50% of tumor cells; GFAP was negative. Findings confirmed a high-grade oligodendroglioma originating within the optic chiasm and nerves. No metastases were observed.
Limitations
As a single case report, findings cannot be generalized. The initial biopsy was nondiagnostic, and no therapeutic interventions were attempted, preventing evaluation of treatment response. The rarity of canine optic pathway oligodendrogliomas limits comparative interpretation, and molecular characterization analogous to human glioma classification was not performed.
Conclusions
This case documents the first known high-grade oligodendroglioma affecting the optic chiasm and bilateral optic nerves in a young dog. The tumor’s location, limited intra-axial involvement, and clinical presentation suggest a primary optic pathway origin—distinct from typical intracranial oligodendrogliomas. The case parallels rare pediatric human optic pathway oligodendrogliomas and underscores the need for further molecular characterization of canine gliomas to refine diagnosis and advance comparative oncology.
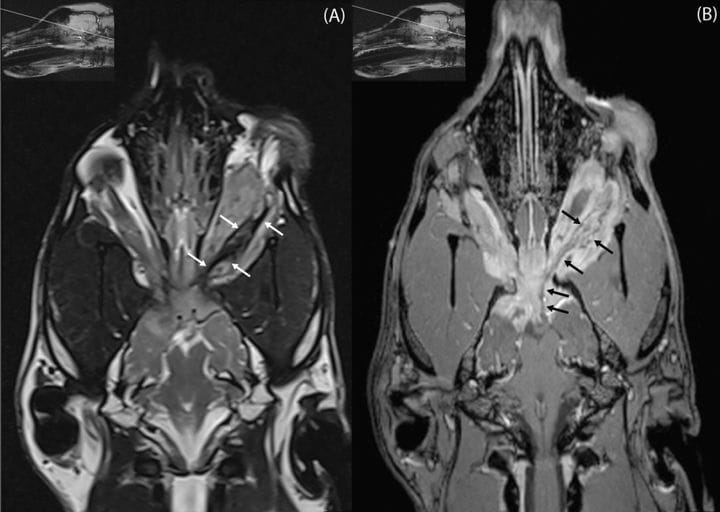
High-resolution images focused on the optic nerve with insets showing the exact imaging plane. (A) T2-weighted dorsal plane image optimized for the optic nerve. Small white arrows outline the retrobulbar portion of the mass encasing the optic nerve, which displays a focal, ill-defined hypointense thickening mid-aspect. (B) T1-weighted post-contrast dorsal plane image optimized for the optic nerve, acquired at a level just dorsal to (A). Small black arrows trace the enhancing retrobulbar portion of the optic nerve sheath complex extending towards the optic chiasm.
How did we do? |
Disclaimer: The summary generated in this email was created by an AI large language model. Therefore errors may occur. Reading the article is the best way to understand the scholarly work. The figure presented here remains the property of the publisher or author and subject to the applicable copyright agreement. It is reproduced here as an educational work. If you have any questions or concerns about the work presented here, reply to this email.