- Veterinary View Box
- Posts
- New Study: Clean Surgical Margins Key to Survival in Dogs with Spinal Nerve Sheath Tumours
New Study: Clean Surgical Margins Key to Survival in Dogs with Spinal Nerve Sheath Tumours
Frontiers in Veterinary Science 2025
Jonathan Deacon, Jos Bongers, and Catherine Stalin
Background
Peripheral nerve sheath tumours (PNST) are uncommon soft tissue sarcomas of Schwann cell or perineural origin, accounting for about 2% of all canine neoplasms. These tumours frequently cause chronic pain, lameness, or paresis, particularly when affecting the brachial or lumbosacral plexuses. Surgical excision is considered the only effective treatment, but achieving complete (R0) margins is technically challenging due to proximity to the spinal cord and vital structures. This study retrospectively evaluated the outcomes of dogs undergoing surgical treatment for spinal PNSTs over a 10-year period, focusing on survival, recurrence, and factors influencing prognosis.
Methods
A single-centre retrospective cohort study was conducted at Moorview Referrals (UK) on 18 dogs with histologically confirmed PNSTs treated between 2014 and 2023. Inclusion criteria required a confirmed diagnosis, detailed clinical and imaging data, and at least 12 months of follow-up. Data collected included clinical presentation, imaging findings (CT and MRI), surgical method, complications, histopathology, and survival time. Surgical techniques included compartmental resection, amputation, and combinations with laminectomy, durectomy, or rhizotomy. Tumours were graded according to a modified FNCLCC histological classification, and surgical margins were categorized as R0 (complete) or R1 (microscopic residual). Survival outcomes were analyzed using Kaplan–Meier curves.
Results
Eighteen dogs (median age 8 years, range 6–12 years) were included, with Labrador Retrievers overrepresented (44%). The most common presenting signs were lameness and muscle atrophy (83%), often with chronic progression. Tumours primarily involved the brachial (61%) or lumbosacral (22%) plexuses. Surgeries performed included compartmental resections (n=9), amputations (n=8), and hemipelvectomies (n=2).
-Tumour grades: 37% grade 1, 47% grade 2, 16% grade 3.
-Margins: 32% R0, 68% R1.
-Median survival time (MST): 326 days (range 28–1,374 days).
-R0 margins: Median survival 850 days vs. 217 days for R1 (p=0.007).
Tumour grade did not significantly influence survival (p=0.099). Postoperative complications occurred in 28% of dogs (mostly mild), and 94% survived to discharge. Three dogs remained alive at study completion. Most non-amputated patients (67%) showed improved limb function postoperatively, while 33% remained stable.
Limitations
The study’s retrospective design and small sample size limited statistical power and the ability to control for confounders. Histopathological grading and margin assessment were performed by different pathologists over time, introducing variability. Client selection bias and breed overrepresentation (especially retrievers) may have influenced findings. Follow-up periods varied, and adjunctive treatments (chemotherapy, radiotherapy) were inconsistently applied.
Conclusions
Surgical management of canine spinal PNSTs, particularly when clean (R0) surgical margins are achieved, significantly improves survival and comfort. Tumour grade had minimal prognostic value, while margin status was the strongest predictor of outcome. Although amputation and extensive resections can provide curative margins, even palliative surgeries yielded improved function and quality of life. Future prospective, multi-centre studies with standardized grading and follow-up are needed to refine prognostic indicators and optimize surgical decision-making for canine PNSTs.
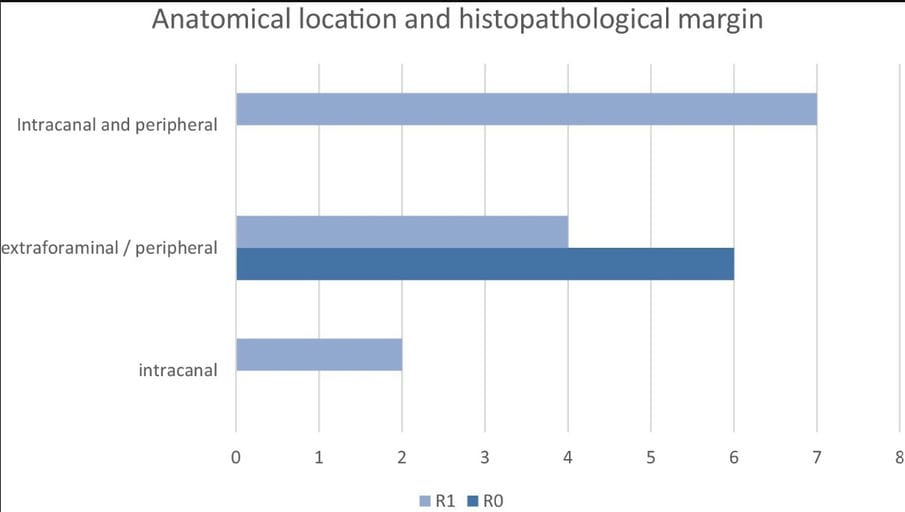
. Anatomical location and histopathological margin.
How did we do? |
Disclaimer: The summary generated in this email was created by an AI large language model. Therefore errors may occur. Reading the article is the best way to understand the scholarly work. The figure presented here remains the property of the publisher or author and subject to the applicable copyright agreement. It is reproduced here as an educational work. If you have any questions or concerns about the work presented here, reply to this email.