- Veterinary View Box
- Posts
- Should we repeat MRI in MUE cases?
Should we repeat MRI in MUE cases?
J Vet Intern Med. 2025
Rita Gonçalves 1 2, Gemma Walmsley 1 2, Thomas W Maddox 1 2
Background
Meningoencephalitis of unknown origin (MUO) encompasses a group of suspected immune-mediated CNS diseases in dogs, including granulomatous meningoencephalitis (GME), necrotizing meningoencephalitis (NME), and necrotizing leukoencephalitis (NLE). While magnetic resonance imaging (MRI) is pivotal for diagnosis, it was unclear whether MUO leads to brain atrophy and whether such atrophy correlates with clinical outcomes.
Methods
This retrospective study analyzed 23 dogs diagnosed with MUO who underwent two brain MRIs at least six months apart using the same imaging equipment. MRI variables assessed included interthalamic adhesion thickness to brain height ratio (ITr), lateral ventricle to brain height ratio (LVr), ITr/LVr, bicaudate ratio (BCR), and total parenchymal brain volume (TPBV). Neurological status was quantified using the neurodisability scale (NDS), and cerebrospinal fluid (CSF) analysis was also conducted.
Results
All MRI-derived measures showed significant changes over time, suggesting progressive brain atrophy. TPBV decreased significantly, and lower TPBV was associated with reduced survival. LVr correlated with higher NDS scores at follow-up, indicating more severe neurological deficits. Although 13 dogs experienced clinical relapse, no specific MRI variable was predictive of relapse. Six dogs developed new lesions on repeat MRI, and most of these dogs later relapsed. Only one follow-up MRI was considered normal, and contrast enhancement was observed in four cases, all of whom later relapsed or had progressive disease.
Limitations
The study lacked a healthy control group to distinguish disease-related changes from normal aging. MRI intervals and treatment regimens were not standardized. Small sample size and the retrospective design further limited the strength of conclusions. Post-mortem confirmation was unavailable, and MRI-based subtype classification may not be fully reliable.
Conclusions
Brain atrophy likely occurs in dogs with MUO and is associated with poorer outcomes, including decreased survival. MRI can detect subclinical disease progression, especially through new lesions and contrast enhancement, which may warrant more aggressive treatment strategies. Repeated MRI evaluations may be valuable for monitoring MUO despite clinical remission.
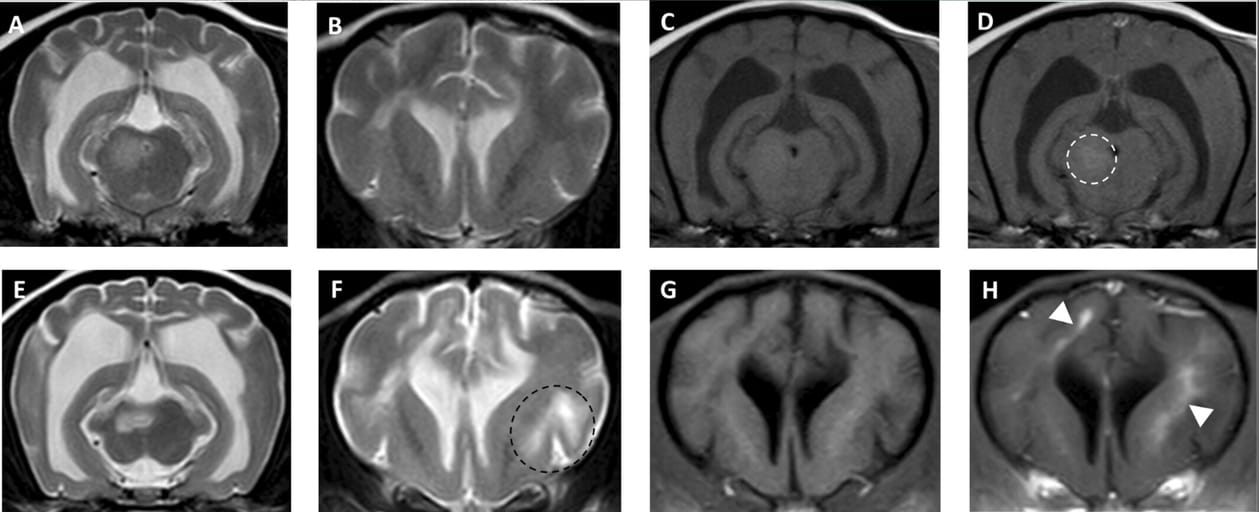
Magnetic resonance imaging of a 3-year-old crossbreed with MUO that showed clinical improvement but remained with permanent neurological deficits at the time of initial diagnosis of MUO (A–D) and 12-months later (E–F). Images (A–B) and (E–F) are transverse T2-weighted (T2W) images, showing enlargement of the lateral ventricles and sulci, suggesting parenchymal atrophy and also development of a new lesion in the frontal cortex (black dotted circle) not seen in the initial MRI. Images (C) and (G) are transverse T1-weighted (T1W) images and (D) and (H) are transverse T1W post-contrast images showing the only mildly contrast enhancing lesion in the initial MRI (dotted white circle) and the new areas of contrast enhancement in the second MRI (white arrowheads).
How did we do? |
Disclaimer: The summary generated in this email was created by an AI large language model. Therefore errors may occur. Reading the article is the best way to understand the scholarly work. The figure presented here remains the property of the publisher or author and subject to the applicable copyright agreement. It is reproduced here as an educational work. If you have any questions or concerns about the work presented here, reply to this email.